Популярное
Полезные советы

Важно знать!
1,1-диметилгидразин
Иприт: последствия, формы поражения ядовитым газом
Основное действие иприт оказывает на глаза, дыхательные пути, кожу. Если отравляющее вещество распыляется в форме газа, то воздействие газа иприта на...
Читать далее
7 безобидных повседневных вещей, которые могут нас убить
10 очень откровенных фильмов о любви и страсти
29 февраля: какой знак зодиака — рыбы
5 грандиозных тайн, раскопанных археологами на алтае
8 ноября
15 способов нарисовать мультяшную и реалистичную мышку
6 фильмов про алтай, которые стоит посмотреть
1 рубль 1961 года. цена и разновидности
7 уровней иерархической пирамиды американского социолога маслоу
Рекомендуем
Лучшее

Важно знать!
2020 год
Каким будет високосный 2020 год
Еще с давних времен в народе закрепилось чувство острой нелюбви к високосному году. Люди стали замечать, что такие годы оставляют по себе дурную славу. Происходят природные...
Читать далее
10 интересных фактов о марианской впадине — самом глубоком месте на земле
5 лучших торговых марок красной икры по мнению роскачества
9 полезных свойств знаменитого алтайского чая для чистки сосудов
12 августа
11 причин, почему японцы носят маски на лице
20 лет у власти. достижения и провалы путина
7 советов по выбору бани-бочки: виды, преимущества, недостатки
8 лучших сайтов для самообразования: сделайте из себя гения
25 лет без владислава листьева: факты и версии, кто его убрал
Новое
Обсуждаемое

Важно знать!
100 рублей чемпионат мира по футболу 2018: новая памятная банкнота
Другие памятные 100-рублевки — общие черты и отличия
Банкнота, выпущенная к ЧМ 2018, не стала первой памятной купюрой современной России. Несколькими годами раньше в Сбербанк и другие кредитные учреждения...
Читать далее
1976 год какого животного в восточном календаре
8 деталей весеннего гардероба женщин после 45 лет, которые освежают образ
15-летние школьницы устроили на камеру секс-насилие над голой сверстницей
7 самых любопытных фактов о взаимоотношениях человека и кошки
1956 год: характеристика огненной обезьяны, совместимость с другими знаками
5 овощей, которые полезнее есть сырыми
18 самых известных спортсменов-геев
5 леденящих душу фактов про обычных крыс
90-е: десятилетие, которое нас объединило 6-я серия — «обратный отсчёт»
Актуальное
Важно знать!
День матери в 2020 году — какого числа праздник всех мам
Конкурсы
Портрет мамы Детям раздаются принадлежности для рисования: карандаши, краски, фломастеры, листы бумаги. Используя свою фантазию, дети должны нарисовать портрет мамы. Готовые работы выставляются...
Читать далее
История дня матери в россии
Выходной или рабочий день 30 декабря 2019 года
День юриста
Новый год 2020: как встречать, что приготовить на праздник
День бухгалтера 2019 в украине: когда и как отмечается
День конституции рк: поздравления с праздником
Влад бумага а4
Год свиньи гороскоп, 2019 год какого животного
Поздравления коллег с днем бухгалтера своими словами
Обновления
 Без рубрики
Лучшие виды Москвы: увлекательные экскурсии на вертолете!
Без рубрики
Лучшие виды Москвы: увлекательные экскурсии на вертолете!
Город Москва, как историческая и культурная столица России, предоставляет уникальные возможности для...
 Новости барнаула
Новости барнаула
Покровский кафедральный собор
Мы уже знаем, где находится г. Барнаул. Расскажем про еще одну его достопримечательность....
 День конституции рф: когда и что за праздник? 12 декабря — выходной или нет?
День конституции рф: когда и что за праздник? 12 декабря — выходной или нет?
Новогодние выходные в РФ 2020
Весь список праздников может не совпадать от одного региона к другому....
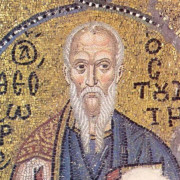
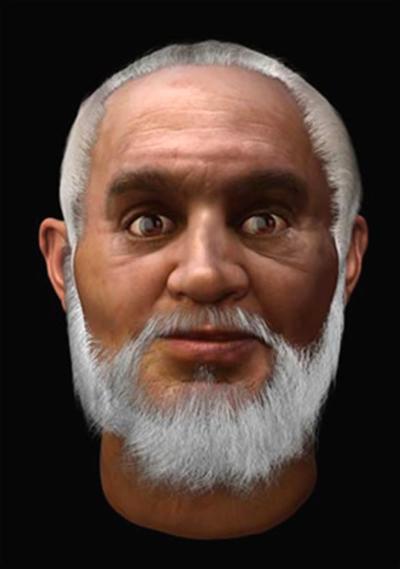 Святой николай чудотворец и николай угодник: в чём разница?
Святой николай чудотворец и николай угодник: в чём разница?
Правда ли, что иконы практически точно передают облик святителя?
Профессор Луиджи Мартино (справа)...
 Насколько опасны серые крысы и почему они заводятся?
Насколько опасны серые крысы и почему они заводятся?
Морфология
Длина тела до 275 мм, хвоста – до 195 мм. Хвост короче тела, что особенно характерно для...
 Пасха 2020: как высчитать дату пасхи в 2020 году
Пасха 2020: как высчитать дату пасхи в 2020 году
Как отмечают Пасху в России и мире
К Светлому воскресенью в нашей стране готовятся заблаговременно....
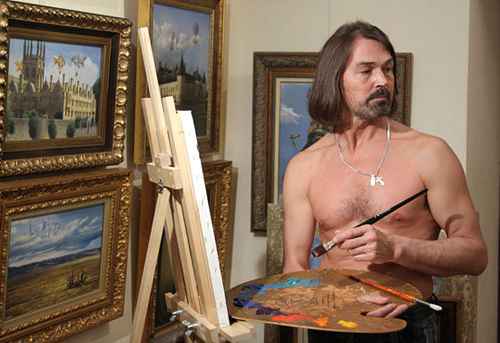 Как похудел сын никаса сафронова
Как похудел сын никаса сафронова
Детство и юность
Никас Степанович Сафронов (настоящее имя — Николай) родился 8 апреля 1956 года (знак...
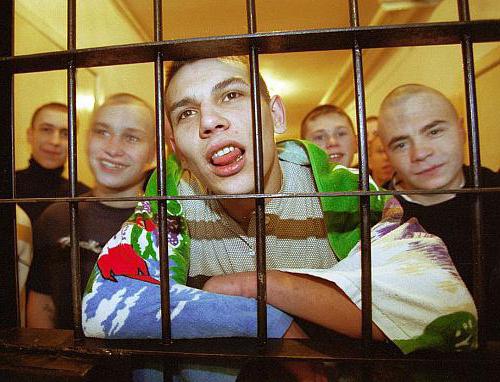 Что значит «ауе»: история, события, расшифровка
Что значит «ауе»: история, события, расшифровка
В кино, литературе и музыке
И всё-таки большинству обычных граждан все эти тюремные реалии знакомы,...
 Сандра баллок
Сандра баллок
Биография
Сандра Буллок – одна из самых высокооплачиваемых актрис Голливуда, владелица собственной продюсерской...
 Киномир барнаул
Киномир барнаул
Человек-невидимка
Жанр: фантастика, триллер.Режиссер: Ли Уоннелл.
В главных ролях: Элизабет Мосс, Оливер...
 Бэдкомедиан
Бэдкомедиан
Реальная сказка
Ладно, вернёмся ненадолго в светлую эпоху раннего БэдКомедиана, когда удачных обзоров...